Periacetabular Osteotomy for Hip Dysplasia in a NCAA Division I Female Water Polo Athlete
Article information
Abstract
OBJECTIVES
The purpose of this study is to investigate the effect of applying a very minimal weight bearing in the early phase of a general rehabilitation program for returning to sports after periacetabular osteotomy for developmental dysplasia of the hip in physically active populations.
METHODS
A 22 year-old NCAA Division I female water polo player, with no prior history of hip injury and no signs of developmental dysplasia of the hip (DDH), reported to athletic training facility early season complaining of right hip pain after stationary bike workout. The athlete reported hearing and feeling a sudden “pop” within the right hip with immediate hip pain when she was pedaling at moderate intensity of a stationary bike. Numbness and tingling was felt initially with the mechanism. Tender to palpate at the right hip flexor and anterior hip joint, as well as the greater trochanter. The athlete’s chief complaints were pain with walking and prolonged sitting. Antalgic gait noticed during evaluation. A 6-, 12-, and 24-week rehabilitation protocol were performed.
RESULTS
X-ray and MRI images showed no avascular necrosis or fracture. An abnormal alpha angle found and no bursitis or tendonitis was shown. A periacetabular osteotomy (PAO) was performed to rotate the acetabular fragment into optimal position and fixed to the pelvis with 3 screws. During the initial 6-week of post-surgical rehabilitation, the level of pain and edema were minimized, the athlete was able to perform toe-touch and partial weight-bearing with crutches, and restored hip ROMs. From 6 to 10 weeks, the athlete recovered full hip ROMs and able to perform lunges, leg press, deadlifts, mini squats back to pre-injury status. The athlete was able to return to activities of daily living (ADLs) after 12 weeks. At 24 weeks, the athlete was able to fully participate in sports without limitations.
CONCLUSIONS
This case describes the rehabilitation program employed following PAO for an atypical case of DDH in a water polo athlete who had no signs and symptoms of DDH prior to sports participation. At the end of the season, the athlete opted to undergo PAO given the risks and underwent a 6-month rehabilitation before a full return to function. This case report aides with treatment knowledge and postsurgical rehabilitation techniques for athletic trainers.
Introduction
An estimated 20-50% of hip degeneration cases are secondary to developmental dysplasia of the hip (DDH), however the exact etiology of DDH is unknown [1]. Interestingly, DDH occurs more frequently on the left side than the right due to the position of the fetus during the last third period of pregnancy [2-4], and approximately 4 times more frequently occurs in girls than in boys due to ligament laxity by maternal hormones [2], and also it’s more involved in Caucasians [5]. This disorder usually identified in infancy, though many cases remain asymptomatic until much later in adult life [3,4]. It occurs when the acetabulum is too shallow and the femoral head is insufficiently covered. This results in lateralization of the femoral head on the acetabulum, and subsequently increases the stress on the outer edge of the acetabulum. Generally, the dome of the acetabulum is subject to the most pressure whereas there is virtually none placed on the acetabular rim. In dysplastic hips, however, this dynamic is altered and increased pressure is placed on the labrum of the shallow acetabulum. Repetitive stress on this edge can lead to hip pain, labral tears and ultimately increase the risk for early onset of osteoarthritis of the hip joint. Though there is a strong association of labral pathology with DDH, not all cases are evident of labral injury [6].
Periacetabular osteotomy (PAO) has become the leading procedure to treat symptomatic DDH [7]. It is the most commonly used procedure because it allows for reorientation of the acetabulum without excessively compromising or damaging the surrounding musculature and blood supply [7]. Furthermore, the posterior column of the pelvis remains stable, allowing for partial weight-bearing immediately after surgery. PAO is shown to improve hip pain associated with DDH, as well as delay the onset of hip osteoarthritis. With this technique surgeons can normalize joint pressures and decrease stress placed on the labrum along the acetabular rim [7]. Studies by Ganz et al [8] and Troelsen et al [9] have illustrated favorable outcomes from PAO, even after longterm follow-up.
The purpose of the study was to discuss on diagnosis, management, treatment and outcome of a classic presentation of DDH fixed with PAO patients and to apply an effective rehabilitation protocols for returning to sports after PAO for DDH in physically active populations without having existing signs and symptoms.
Case Presentation
The patient was a 22 year-old NCAA Division I female water polo athlete (height: 176.5 cm; mass: 70.3 kg). Mechanism of injury was working out on a stationary bike, the athlete felt “pop” within the right hip with immediate sharp pain. Complained of some initial numbness and tingling sensation felt around the hip. No prior history of hip pain with suspecting labral tear or hip subluxation. The athlete reported pain with walking and sitting, and an antalgic gait was observed. Active range-of-motion (AROM) was decreased significantly, specifically in hip flexion, abduction, and external rotation, all limited by pain. Passive range-of motion (PROM) was limited in hip flexion and abduction with pain. Hip abduction and flexion isometric strength was 4 out of 5 with pain; 4 out of 5 hip external rotation and internal rotation without pain. Tender to palpate at the right hip flexor and anterior hip joint, as well as the greater trochanter. Special tests included FADDIR (hip flexion with adduction and internal rotation), otherwise known as the impingement test positive; FABER (hip flexion with abduction and external rotation) test positive for labral pathology; Ely’s test positive for hip flexor tightness; Thomas test negative for quadriceps tightness; Kendall’s test positive for hip flexor tightness. Referred to the team physician for further examination and sports practice or participation was immediately discontinued.
The patient received magnetic resonance imaging (MRI) for the right hip to evaluate a labral tear, causes of pain and popping. Coronal Short Tau Inversion Recovery (STIR) images of the pelvis in addition to coronal and oblique axial proton density (PD), axial PD (Fat Sat), and sagittal PD (Fat Sat) images were taken of the right hip. Findings showed no avascular necrosis or fracture. The proximal femoral shafts were normal and no bone edema found. There was a small amount of the hip joint fluid bilaterally similar in amount to the left side more anteriorly on the right side and more posteriorly on the left side. There was no cartilage or subchondral abnormality of either hip joint. Ligamentum teres was intact bilaterally. The lateral center edge angle (LCEA, Wiberg angle), an angle formed by the perpendicular to the inter-tear drop line and the line from the center of the femoral head to the lateral edge of the acetabulum [10,11], was borderline shallow 22° on the right side <Figure 1>. There was a tear along the base of the anterior labrum with a shallow detachment best appreciated axial 9 oblique axial 8 and 9. There was no posterior labral tear or lateral labral tear. Mild osseous ridging along the anterior femoral head neck junction found and no acetabular retroversion showed. All tendons about the right hip joint as well as remaining pelvis are intact. There was no soft tissue calcification, bursal collection or focal soft tissue edema. Muscles around pelvis were normal. No subchondral or cartilage abnormality, but had a borderline shallow acetabular coverage. Abnormal alpha angle found with no bursitis or tendonitis revealed. Seven months later, PAO was performed to rotate the acetabular fragment into optimal position and fixed to the pelvis with 3 screws <Figure 2>.
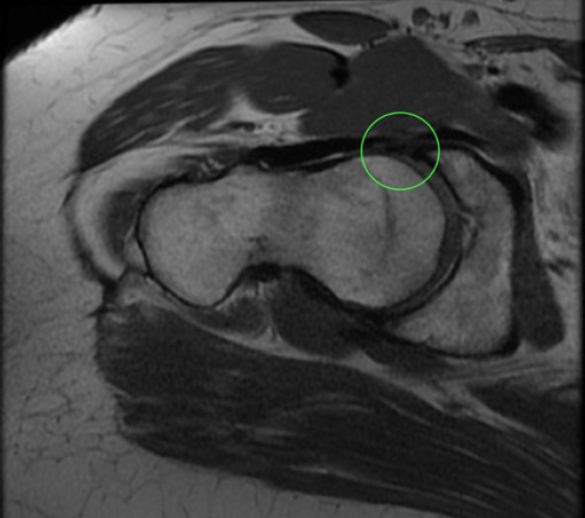
MRI showed the center edge angle is borderline shallow 22° in the right hip, a shallow acetabular coverage. A tear located along the base of the anterior labrum with a shallow detachment.
Intervention
Brief Operative Note
An epidural was placed by the anesthesiologist for intraoperative and postoperative pain control. The patient was given a general anesthetic and was then given prophylactic IV antibiotics. An oblique bikini incision measuring approximately 8 to 10 cm was made starting distal and lateral to the anterior-superior iliac spine (ASIS) and directed inferomedially, passing directly over the hip joint. The sheath of the tensor fascia latae was divided longitudinally and this muscle was retracted laterally. The sartorius was sharply detached from the ASIS. The inner table of the ileum was elevated with the iliacus retracted medially into the pelvis. Exposure of the superior ramus of the pubis was completed using electrocautery and a Cobb elevator. Dissection was continued medially over the pubic eminence until Kregel retractors safely passed around the bone at the obturator foramen. Scissors were introduced into this region and used to palpate the ischium in the region just inferior to the acetabulum. At this point, all three areas of the later osteotomy were exposed. An oscillating saw was used to make the third osteotomy in the ileum. The ileum was cut bicortically without any stripping of the lateral musculature off the outer table. The entire osteotomy propagated and the acetabulum was then entirely mobilized. For fixations, a large threaded Schantz pin was then placed into the supra-acetabular bone for mobilization and control of the acetabular fragment. Anterior impingement was tested for by flexing the hip to greater than 90°. The amount of femoral anteversion was carefully assessed by looking at the anterior and posterior wall radiographic lines for evidence of a cross-over sign. The osteotomy in place with three 2.8 mm smooth Steinman pins, which were then switched out for Synthes 4.5 mm fully threaded cortical screws. The lateral corner of the osteotomy was then trimmed so it was not prominent and used as bone graft in the osteotomy site. The patient was successfully extubated and sent to recovery in a stable condition.
Post-Operative Rehabilitation Protocol
Complications to watch out for wound infection, deep vein thrombosis, non-union of the bone, leg length discrep-ancy, loosening of fixation, and/or neural damage were observed. Initial goals of rehabilitation (0- to 6-week) were pain and edema control, education of partial weight-bearing and restoring partial hip ROMs by the 6-week.
Use of Crutches
The patient was instructed how to walk non-weightbearing correctly with crutches. From the postoperative day 2, toe touch weight bearing with crutches for 6 weeks, the only time flat-footed weight-bearing was permissible when patient was able to stand with crutches, though no (very minimal) weight bearing applied to the injured side. Flat-footedness was permitted when standing on crutches for balance only (approximately 20% weight-bearing), no (very minimal) weight-bearing on the right side to ensure the fixation screws remain intact. No planned exercises for the 1st 6 weeks to protect acetabular position and screw fixation except ROM exercises. From 6- to 8-week, the patient gradually progressed from toe-touch to partial to full weight bearing using crutches. From 8- to 10-week, one crutch was used, the patient did not use crutches and demonstrated non-antalgic gait by the 10-week.
ROM Exercises
There was no ROMs restriction, though as a precaution, hip flexion limited to 80-90°, hip internal and external rotation to 15-20°, and hip adduction and abduction to 15-20°. Supine hip ROM exercises were performed while standing hip ROM exercises were restricted. At 4 weeks, the patient was able to walk in water with caution and perform aquatic exercises to help restore gait and lower extremity pain-free ROMs. Along the basic caution the above, physical therapy was performed from the 6-week and required to fully rehabilitate the surgically repaired hip. From 6- to 10-week, the patient’s radiographic evidence showed healing and union of the bone, and exercise progressed to full weight-bearing permitted with pain free ROMs. The hip ROM exercises performed passively and gently at this phase, and included knee ROM exercises and the patient encouraged to perform the knee ROM exercises actively. In addition, exercises include clinician-assisted soft tissue mobilization techniques for the hip ROMs. Gravity eliminated hip ROM exercises were initiated and pain-free hip normal ROMs were slowly gained and weight bearing hip ROM exercises between 10- to 12-weeks. At 12-week, pain-free full hip ROMs restored and continue to perform weight-bearing hip ROM exercises as tolerate up to 5 months.
Strengthening Exercises
Between 6- to 8-week, isometric strengthening of the hip and quadriceps, ankle mobility, ankle related muscle strengthening, and balancing with crutches were initiated while exercises focused on pain-free hip ROMs, strength and eventually proprioception and stability exercises were performed as well. The patient started riding a stationary bicycle with the seat elevated to avoid straining the hip joint. Early on, isometric as well as concentric and eccentric muscle contractions were performed to restring muscle strength. Open kinetic chain (OKC) exercises were prescribed and performed, considering the patient was not fully weight-bearing yet during the exercises. Quad set isometric contractions and/or ankle pumps (dorsiflexion and plantarflexion) were performed. During this period, the patient performed proprioceptive and stabilization exercises such as a single leg stance. In addition, core strengthening exercises introduced to incorporate lower extremity with the rest of the kinetic chain exercises. When the patient was able to fully support her weight without pain, she performed closed-chain activities or closed-kinetic exercises. Exercises included deadlifts, standing squats or lunges, and leg press. Gait re-education was introduced during this period. We encouraged independence of the patient with home exercise programs and continued adherence to the exercise rehabilitation.
Resistive elastic tubing exercises were initiated and continue to restore normal hip strength through 10- to 12-week. At 5-month, full hip strength restored.
Additional Activities/Sports-Specific Exercises
From 6- to 12-week, the patient performed proprioceptive and stabilization exercises such as a single leg stance. In addition, core strengthening exercises introduced to incorporate lower extremity with the rest of the kinetic chain exercises. When the patient was able to fully support her weight without pain, she performed closed-chain activities of daily living (ADLs) and closed-kinetic exercises. Exercises included deadlifts, standing squats or lunges, and leg press. Gait re-education was introduced during this period. We encouraged independence of the patient with home exercise programs and continued adherence to the exercise rehabilitation.
At 12 weeks and beyond, the patient was able to return to ADLs, from typical to pre-surgery activity status. Core strength, proprioception and functional activity were emphasized in this period. Given the case subject was a collegiate athlete, exercises became more sport specific. Normal gait restored without compensation and completely independent of walking aides. Continued to increase lower extremity strength and core strength as well. Approaching 5 months, the patient was able to return to regular sporting activities without limitations. Resistive exercises gradually progressed from 10- to 12-week to 5-month, From 12-week, hip muscle strengthening exercises using 3 axes and planes of the hip joint were performed while weight bearing and additional resistance, and stationary bike riding was also performed by lowering the seat height with adding resistance. Muscle strength, power, and endurance exercises were performed while increasing intensity, frequency, and duration of the exercises gradually. Jogging and running exercises were added, and sport-specific exercises for water polo were performed both on land and in water.
Post-Operative Follow Up Care
The care schedules were as follows:
1. Two weeks post-op: Wound and incision check.
2. Six weeks post-op: X-rays to assess the bone healing and progression to full weight-bearing.
3. Three months post-op: Further x-rays as well as discuss activity modification and progression.
4. Five to six months post-op: Further x-rays and status update.
Discussion
The water polo athlete was asymptomatic prior to injury. Upon further examination and diagnostic imaging, discovered borderline DDH on right side. Shallow detachment of the anterior labrum from the acetabulum also associated with injury. Hip dysplasia was not originally suspected. This case study demonstrates the typical presentation [1,7,10], diagnosis [2,11,12], post-operative plan [2,6] and care, and rehabilitation program for DDH patients. The athlete presented with classic symptoms for DDH and associated labral pathology: hip pain with flexion, clicking, and positive FABER and impingement special tests. However, this water polo athlete had no signs and symptoms, but it was characterized by a sudden incidence during a general warming up. PAO is one of the most common surgical procedures used to fix hip dysplasia though in less documented in an athletic population [3,10-12].
In this case study, the athlete’s LCEA was 22°, which is a typical lateral dysplastic corresponding to 60.4% of the data reported by Dornacher et al [10] among 192 PAO patients and agreed with a similar study was conducted by McClincy et al [11]. In the Hartig-Andreasen et al [12] study found that labral tear was previously reported to be more than 90% complaining of the hip joint pain, but at present, it is reported that external labral tear is not commonly reported, however, a labral tear found in this case athlete.
When sports medicine teams care for athletes, they generally focus on recovery through rehabilitation exercises after injury, but as in this case, athletic trainers should carefully evaluate the pain that occurs in athletes indirectly related with sports injuries as well as the pain that occurs in ADLs. We want to continue follow-up on this athlete, but as the player graduated, we couldn’t follow-up for the next season, so we could only obtain short-term rehabilitation results to report of this unique case.
Conclusion
We asked the athlete to use a very minimal weight-bearing carefully to maintain a stable position of the screwed acetabular in the standing position only at weeks 5 and 6 while relying on crutches, but compared to a typical rehabilitation program in which no weight-bearing was supported at all. It had the similar result of returning to normal life activities at 6 months.
Although there are various roles of athletic trainers to care of the health and assist to reach peak performance of athletes, in reality, it is practically unreasonable to manage all athletes due to the number of athletes and the ratio of athletic trainers. In this case, due to the nature of water polo sport, a player who had no symptoms despite constantly using the hip joint tremendously against the water to stay afloat was unable to continue the season due to symptoms appearing during a general warm-up exercise. Despite the practical difficulties described above, it is recommended that athlete trainers evaluate and assess athletes through pre-participation examinations and periodic sports-specific functional tests to find unexpected injuries even without having the most common early signs and symptoms of the injuries.

