Physical Activity and Immunity in the Elderly for the Post-COVID-19 Pandemic Era: A Literature Review
Article information
Abstract
OBJECTIVES
This study aims to summarize previous studies on the relationship between regular physical activity and the immune system in the elderly, and discuss optimal exercise modes to maintain immunity in preparation for novel infectious diseases that may continue to appear.
METHODS
This study referred to the academic papers based on the electronic database, and they were searched using the following keywords: physical activity, immunity, elderly, and COVID-19.
RESULTS
The elderly are more vulnerable to infectious disease such as the novel coronavirus disease 2019 (COVID-19) than other age groups because of lower physiological function and immune surveillance, consequently leading to higher severity of and mortality. Many studies on physical activity and immunity have confirmed that regular physical activity enhances immunity in the elderly population. Physical activity can delay immunosenescence and increase immune resilience by maintaining the function of the innate and acquired immune systems. Because the elderly have low physical fitness, physiological function, and immunity, exercise prescription for the elderly must be approached very carefully and in detail, considering various exercise modes such as exercise intensity and amount. As confirmed in previous studies, homebased light physical activity is a convenient, safe, and effective strategy for the health of the elderly.
CONCLUSIONS
In this study, balance training using body-weight is a good method of home-based physical activity for the elderly, because it not only improves immunity by increasing physical fitness but also prevents frequent falls by increasing the balance ability of the lower extremities. Future studies should be conducted on various exercise modes and optimal exercise training to improve immunity in the elderly.
Introduction
The novel coronavirus, which emerged in the winter of 2019, has been a threat to human health for over two years and is still ongoing. This novel coronavirus, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes COVID-19 and is spreading rapidly worldwide. The WHO declared the outbreak a public health emergency of international concern [1]. According to the WHO, most people with COVID-19 have mild symptoms, but some become severely ill. Older adults and those with certain underlying medical conditions are more likely to become severely ill. Some people with COVID-19 experience long-term effects from the infection. These long-term effects cause a wide range of health problems with symptoms, such as dizziness, headache, chest pain, heart palpitations, and musculoskeletal pain [2].
The spread of COVID-19, which has been decreasing according to each country’s control measures, began to take on a new pattern in late 2021. In November 2021, the WHO designated variant B.1.1.529 a variant of concern (VOC), named Omicron. Omicron is a highly divergent variant with a large number of mutations [3]. Unfortunately, the emergence of new variants of viruses that sustain the pandemic is discouraging individuals who hope to return to their daily lives around the world.
Under the WHO’s Pandemic Declaration, many countries have taken social measures such as home-working, social distancing, and wearing of face masks, although these vary from country to country. Although these measures were effective in preventing the spread of the virus, they partially restricted physical activities in the gym and outdoor. Due to social distancing, changes in lifestyle, such as reduced physical activity have been causing not only decreased physical health but also psychological health problems such as anxiety and depression. All these risk factors are the cause of chronic diseases, which can lead to serious health problems for individuals and communities [4,5].
As is well known, lack of physical activity is closely related to increased mortality, as well as chronic diseases, such as type 2 diabetes, and cardiovascular disease [6,7]. Changes in lifestyle (i.e., physical inactivity, excessive eating, and stressful daily life) affect not only non-communicable diseases but also immune functions that prevent infectious diseases. Many studies have reported that regular physical activity is an important non-pharmacological intervention method that can enhance immune function to prevent infectious diseases [8-10]. The elderly are more vulnerable to COVID-19 with increase in severity and mortality due to their low immune surveillance and physiological function [11]. Additionally, the decrease in physical activity due to various measures taken to prevent COVID-19 may further encourage the elderly to lower their physical fitness and physiological function. In the elderly, degeneration of the cardiovascular and respiratory systems, including structural and functional changes in the heart, blood vessels, and lungs, occurs during aging [12].
It is well known that regular physical activity improves immunity in the elderly [13,14], and additionally, some reports suggest that regular physical activity increases vaccination response as well as preventive effect on infectious diseases [15,16]. However, exercise interventions for the elderly must be approached very carefully and in detail because of their low physical fitness and physiological conditions. In particular, there is a lack of research on the relationship between immunity and exercise modes in the elderly, so more studies should be conducted considering various exercise methods to improve the immune function of the elderly in the COVID-19 era. Therefore, this paper aims to summarize previous studies on the relationship between regular physical activity and the immune system in the elderly, and discuss optimal exercise modes to maintain immunity in preparation for novel viruses that may continue to appear.
1. Physical Activity and Immunity in the Elderly
The general consensus among many studies on the relationship between physical activity and the immune system suggests that physical activity beneficially influences immunity [9,10,12,17]. Recent epidemiological studies have demonstrated that regular participants in physical activity showed lower rates of incidence, duration, and intensity of symptoms and risk of mortality from COVID-19 [18-22]. These reports suggest that moderate to high levels of regular activity above 150min/week show distinct beneficial effects compared to a low level of physical activity. Regular moderate physical activity leads to beneficial changes in the immune system through improved immune surveillance by providing an increase in the anti-pathogenic activity of macrophages as well as an increase in circulating immune cells (i.e., natural killer cells, neutrophils, lymphocytes, and immature B cells) and anti-inflammatory cytokines, consequently reducing the risk of lung damage due to influx of the novel coronavirus [20,23,24].
The degree of infection with SARS-CoV-2 is affected by various health-related factors, of which age is considered an important variable. This is because the severity and mortality rate of COVID-19 is the highest among the elderly [24]. Immunosenescence can be described as a deterioration of the immune system resulting from increasing age, and is considered a major cause of lowered immune surveillance, poor response to vaccination, and severity and high mortality associated with infectious diseases [17]. Immunosenescence is a complex aging-related change in the immune system duo to a series of biological events, including a reduction in humoral and cellular immunity, and an increase in inflammatory materials [25]. Aging stimulates the inflammatory process by increasing the secretion of pro-inflammatory cytokines (i.e., interleukin-1 (IL-1), tumor necrosis factor-alpha (TNF-α), IL-6, and C-reactive protein (CRP)) [9]. With aging, macrophages promote an inflammatory response that releases large amounts of TNF-α, IL-12, which can accelerate tissue damage [24].
Given the known positive effects of physical activity on immunity in the elderly, regular physical activity has been proposed as a reliable therapeutic strategy to mitigate the effects of aging on the immune system and offset the harmful effects of immunosenescence. More precisely, planned exercise considering the functional and physical level of the elderly is more effective than daily physical activity. This is well supported by a number of epidemiological and experimental studies in the elderly, indicating that participation in regular exercise reduces oxidative stress associated with aging and frequency of various immune biomarkers associated with decreased immunity [24,26-28]. This suggests that regular exercise in the elderly can delay the onset of immunosenescence and reduce the risk of infection by novel viruses such as SARS-CoV-2 [17].
Vaccines are one of the key public strategies for preventing COVID-19. Although vaccine-induced immunogenicity may be low in the elderly, regular exercise has also been shown to improve response to vaccination [29,30]. Gualano et al. (2022) reported that when COVID-19 vaccine is administered to individuals who have usually performed physical activity (> 150 min/week of moderate to vigorous intensity), they showed greater improved immunogenicity and higher antibody persistence compared to sedentary people [31,32]. They suggested that physical activity enhances immunogenicity for the SARS-CoV-2 vaccine and sustains its effects over time.
2. Exercise Modes and Immunity in the Elderly
In general, regular or chronic physical activity that affects human systems is called “exercise training”, which can be defined as the repeated bouts of exercise during a short or longterm period. Many reports indicate that exercise training is an effective intervention that reduces immunosenescence and chronic inflammation, and it enhance the improvement of immunity and effectiveness of influenza vaccination in the elderly [33-35]. It is well known that adaptation of the immune system to exercise training depends on exercise modes, such as exercise type (i.e., endurance training, resistance training, etc., time, and intensity (low intensity (below 40% VO2max), moderate (40-69% VO2max), vigorous (70-90% VO2max)) [25]. Exercise types can generally be divided into endurance training, such as brisk walking, jogging, swimming, cycling, resistance training using equipment or body weight without equipment, and flexibility training. Endurance training, which refers to regular aerobic exercise, generally appears to improve the function of the cardiovascular and respiratory systems. Resistance training is commonly used to increase muscular strength and reduce metabolic disease and risk of falling in the elderly [25].
Endurance exercise training, composed of moderate to relatively vigorous intensity workouts (40-70% VO2max), is associated with a lower incidence of upper respiratory tract infection (URTI) [9,25]. These reports supporting the “J-curve” hypothesis showed that URTI incidence was decreased in moderate intensity physical training, but increased in participants in high-intensity training or long-term competitive sports. High intensity exercise (> 85% VO2max) induces transient immunosuppression called “open windows”, which increases susceptibility to infection [23,27]. Shaw et al. (2018) suggested that exhaustive exercise bouts and heavy chronic training changed T-cell immunity to an anti-inflammatory state. This induces impairment of immunity by mounting an inflammatory response to immune challenges, consequently leading to weakened defenses against intracellular pathogens and increasing the risk of infection and viral reactivation [36]. In our previous study on the effect of acute aerobic exercise on immunity in healthy adults, we investigated the effect of different acute exercise intensities on serum leukocytes and lymphocyte subtypes in the exercise amount of 400 kcal, the daily exercise energy consumption recommended by the ACSM [37]. Our study showed that at a high intensity (85% VO2max) of exercise, circulating lymphocytes, and NK cells were reduced to less than the rest level at recovery time after exercise, and T4/T8, the ratio showing immunosuppression, decreased to less than the rest level immediately after exercise. We suggested that low- to moderate-intensity exercise is recommended to prevent systemic immunosuppressive conditions [37]. Furthermore, in another study, long-term high intensity training led to a decline in the ability of innate immune cells to respond to acute challenges, thereby increasing the risk of infection [38].
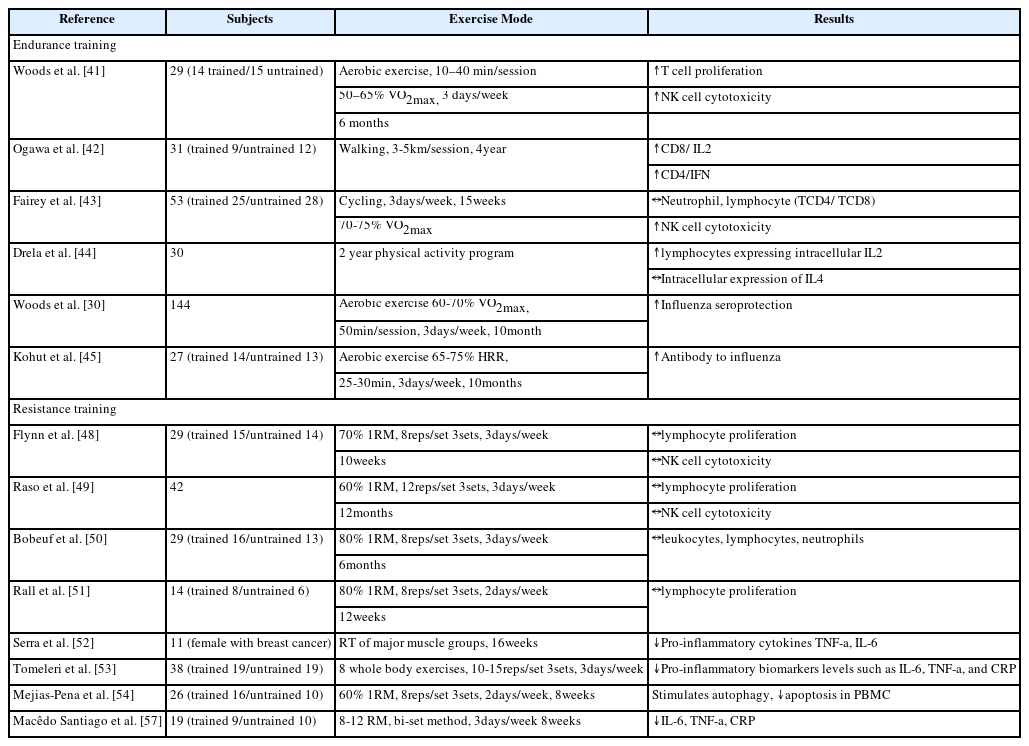
Despite the vulnerability of the immune system to high intensity exercise training, the overall anti-inflammatory effect of regular physical activity can reduce the risk of aging-related chronic diseases characterized by chronic inflammation [39]. Less than 60 min of moderate endurance exercise training have already been proven to have anti-pathogenic activity through improved circulation of immunoglobulin, anti-inflammatory cytokines, neutrophils, NK cells, cytotoxic T cells, and immature B cells, which play important roles in body defense [40-45]. Non-pharmaceutical physical activity interventions may be an important source of immunological protection against novel coronaviruses. Well-managed endurance training may prevent the novel coronaviruses from spreading rapidly from one person to another [46]. According to a recent randomized controlled trial in COVID-19 patients with mild or moderate symptoms, two weeks of moderate aerobic exercise reduced the severity and progression of COVID-19 disorders and increased the levels of leukocytes, lymphocytes, and immunoglobulin A, positively affecting immune function [47]. <Table 1> shows studies about effects of endurance and resistance exercise training on immune functions in the elderly.
Resistance training involves all types of exercises that contract skeletal muscles in response to any kind of force with or without an equipment. Resistance training is one of the various modalities of exercise used to prevent diseases such as cardiovascular disease and type 2 diabetes. However, studies on the effect of resistance training on immunity in the elderly have yielded inconsistent results. Some studies [48-51] have shown that short-term resistance training interventions (8-12 weeks) in healthy elderly individuals (ages 65-84) have no beneficial or detrimental effects (impact count, apoptosis, proliferation, etc.), while other studies [52-54] have found beneficial effects on inflammatory status in patients with breast cancer, metabolic syndrome, or healthy elderly (69 years old). Some studies have reported that resistance training is effective in reducing the serum concentration of pro-inflammatory cytokines (TNF-α, IL-1, and IL-8) [55,56]. One study showed that eight weeks of resistance training reduces the serum concentration of cytokines (IL-6, TNF-α) and C-reactive protein and induces molecular changes in TNF-α gene expression in elderly women. They suggested that this may be related to immunomodulatory and anti-inflammatory effects because resistance training releases myokines (cytokines produced in contracting muscles), particularly IL-6, which acts as a TNF-α antagonist during exercise [57]. These inconsistent results could be due to distinct exercise prescriptions (Type, frequency, intensity, and time), sex and genetic discrepancies.
Structured and progressive resistance training programs can be developed according to the appropriate and specific training purposes for the elderly. Among the various protocols available, the bi-set method demonstrates an efficient proposal for a systematic and individualized resistance training program that follows the resistance training prescription recommendations for the elderly. ACSM and American Heart Association (AHA) recommend that resistance training should be performed for as little as 15-20 minutes a day, 8–12 repetitions, and 60–70% of one-repetition maximum (1RM) on two or three nonconsecutive days per week for the elderly [58,59]. There are various types of resistance exercises such as chest presses, squats, knee extensions, and lunges, but most of these exercises need to be appropriately modified for the elderly [58]. For example, it is recommended that the elderly hold chairs for squats or use elastic bands for chest presses.
3. Practical Alternatives for Daily Physical Activity of the Elderly
The ACSM and WHO, which are authoritative organizations on global health issues, recommend that the elderly actively participate in physical activities to prevent COVID-19 during the pandemic. The WHO recommends that healthy individuals should exercise at least 150 min per week for adults and 300 min per week for children and adolescents. These times should be divided during the days of the week and according to individuals’ lifestyles [60]. The ACSM has also recommended guidelines for moderate intensity activities that can be practiced during the pandemic period, including aerobic exercises and strength training, indoors or outdoors, with permission of government authorities as long as infection prevention measures are maintained [61]. This organization recommends 150-300 min per week of moderate intensity aerobic physical activity and two sessions per week of muscle strength training. Additionally, the ACSM offered several useful tips for maintaining physical activity in older adults at a possible level during the COVID-19 pandemic [62].
Walking is a very useful outdoor activity for improving cardiorespiratory fitness, and exercising in local parks or natural environments, cycling, and gardening are good options for outdoor activities. If it is not possible to exercise outdoors, walking in a place at home, going up and down stairs, dancing to cheerful music, and using home cardio machines, such as stationary cycles, are can be alternatives. [61,62]. The WHO suggested some tips to reduce sedentary behavior and increase active daily life, including having short active breaks during the day, participating in an online exercise class, standing up whenever possible, and using indoor exercise equipment such as stationary bikes and rowing ergometers [63]. The WHO has also suggested examples of home-based exercises to strengthen musculoskeletal and cardiorespiratory fitness, including knee-to-elbow (increasing heart and breathing rates), plank (strengthening core muscles), back extensions (strengthening back muscles), squats (strengthening legs and gluts), side knee lifts (increasing heart and breathing rates), superman (strengthening back, glutes and core muscles), bridge (strengthening gluts), chair dips (strengthening triceps), chest opener (stretching chest shoulders), child’s pose (stretching back, shoulders and sides of the body), legs up the wall (being comfortable, relaxing and de-stressing), and seated meditation (relaxing and clearing one’s mind) [63].
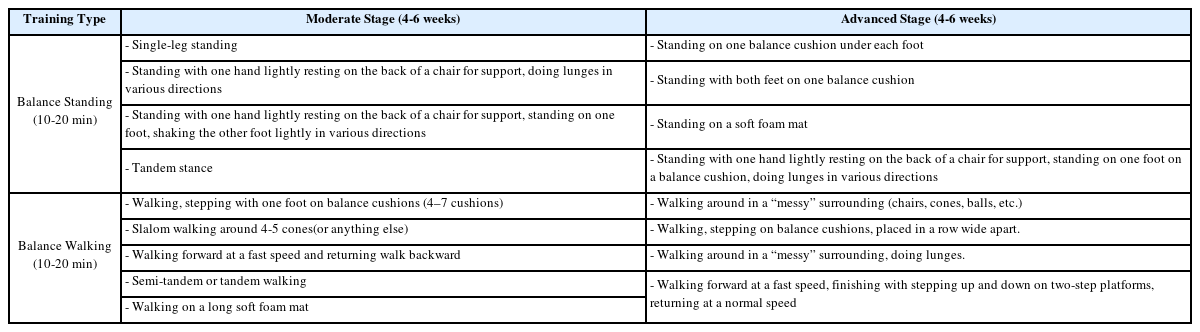
In a previous study, I examined the effects of balance training to improve functional performance in the daily life of the elderly and suggested that balance training improves posture control and balance recovery ability of the elderly [64]. Balance training can be considered a useful homebased exercise program for the elderly in another pandemic era because it can improve various physical fitness, such as muscular strength, as well as balance ability to prevent falls that frequently occur in the elderly [65]. <Table 2> shows an example of some modifications to the proposed home- or community-based balance training programs in my previous study and another study [64,65].
Conclusions
The novel coronavirus, which is assumed to continue to emerge, will continue to affect the daily lives of people around the world. Physical activity must be implemented to maintain everyone’s physical and mental health. In particular, the elderly should practice physical activity regularly to protect their body from infectious diseases. Physical activity in the elderly is an effective way to delay immunosenescence and increase immune resilience by maintaining the function of the innate and acquired immune systems. However, since the physiological function of the elderly has deteriorated, exercise modes, such as exercise intensity and amount should be carefully planned and performed. As confirmed in previous studies, home-based physical activity is a convenient, safe, and effective strategy for the health of the elderly. Balance training using body-weight is a good method of home-based physical activity for the elderly, because it not only improves immunity by increasing physical fitness but also prevents frequent falls by increasing the balance ability of the lower extremities. Therefore, future studies should be conducted on various exercise modes and optimal exercise training to improve immunity in the elderly.
Acknowledgements
This research received no external funding.
Notes
The authors declare no conflict of interest.