Can Low Intensity Strength Training Alone for Older Females Improve Cardiovascular and Functional Fitness?
Article information
Abstract
BACKGROUND
Maintaining muscle mass and an efficient cardiovascular system is vital for healthy aging.
OBJECTIVES
This study investigates if a low intensity senior strength exercise program for the older females can have an effect cardiovascular function and improve senior functional fitness.
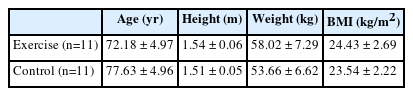
METHODS
There were 22 older females, randomly divided into a strength exercise (age: 72.18 ± 4.97 yrs; height: 1.54 ± 0.06 m; weight: 58.02 ± 7.29 kg; BMI:24.43 ± 2.69 kg/m2) and control group (age: 77.63 ± 4.96 yrs; height: 1.51 ± 0.05 m; weight: 53.66 ± 6.62 kg; BMI:23.54 ± 2.22 kg/m2). The strength exercise group participated three times per week for 20 weeks, while the control group did not do any additional treatment or exercise. Participants were tested pre and post strength exercise, and the data were statistically analyzed using two-way repeated measures Analysis of Variance (ANOVA), with a significance level of p <0.05.
RESULTS
The results show significant differences (p<0.001) in homocysteine levels, with an interaction effect between time and group. There were no differences in changes in erythrocyte sedimentation rate between groups (p=0.050). There was an interaction effect (p<0.001) for the six components of the senior fitness test and between group and time in systolic blood pressure, diastolic blood pressure, heart rate, and pulse pressure.
CONCLUSION
In conclusion the results suggest that low intensity strength exercise program can improved cardiovascular fitness related variables, and homocysteine, as well as functional fitness, blood pressure, heart rate and pulse pressure.
Introduction
Aging is reported to be one of the main causes of reduced physical activity that can lead to diabetes and cardiovascular disease, which are associated with a high death rate worldwide [1]. Increases in blood homocysteine levels are shown to be related to a high risk of coronary artery and cardiovascular disease [2]. Similarly, pulse pressure is an important risk factor for cardiovascular diseases and mortality [3] and it refers to the difference between systolic blood pressure (SBP) and diastolic blood pressure (DBP), an indicator of the elasticity of blood vessels. Aging causes blood vessels to lose their elasticity, become rigid and leads to increases in pulse pressure [4]. This rigidity in blood vessels can cause an increase in SBP and decrease in DBP, dangerously increasing pulse pressure, which leads to complications such as stroke and coronary artery disease [4]. Several studies have shown that increased pulse pressure increases the incidence of stroke, myocardial infarction, and heart failure [5, 6, 7, 8]. Additionally, aging also causes changes in blood pressure, which can reduce functional mobility; thus reducing physical strength by decreased muscle usage [1].
To counteract the negative effects of aging participating in regular exercise is vital for the older in order to maintain health (9, 10, 11), and any experienced exercise instructors must consider sarcopenia while training the older population (12, 13, 14, 15). Furthermore, less muscle mass and reduced function will lead to lower levels of physical activity, which will reduce total energy consumption therefore resulting in a high probability of a weight gain and corresponding rise in the probability of obesity [9]. With the aging associated muscle loss, it is common for the older population to experience joint pain (16, 17), and research has shown that as age increases the probability of joint pain also increases (16, 18). Therefore, due to high levels of joint pain in the older population (16, 17), exercise programs for the older population should be implemented with these issues of muscle loss and joint pain, in mind [12]. As older females tend to suffer from more severe sarcopenia, strength training is particularly important [12]. Even though there is a wide variety of studies portraying the effect of resistance training for maintaining health and controlling hypertension, blood pressure, total and LDL cholesterol [13] there is a lack of studies focusing on older females and resistance training effects on the cardiovascular system. Therefore, for this study we developed a low intensity senior strength exercise program (SSEP) to improve functional fitness for older females.
For convenience and cost effectiveness we integrated the use of plastic bottles as weights. As plastic bottles have an additional advantage in that they are easily accessible the participant can be instructed remotely as well as have the ability to continue to training alone after the strength exercise period. Therefore, the purpose of this study was to evaluate the effectiveness of the SSEP, we investigated the effect of SSEP on homocysteine, total cholesterol (TC), triglyceride (TG), and erythrocyte sedimentation rate (ESR) levels, as well as blood pressure, heart rate, pulse pressure, and senior fitness test (SFT) in older women.
Methods
Participants
Prior to recruitment, the G*power 3.1 program was used to calculate the number of participants needed. Using an effect size of 0.25, an α value of 0.05, and a desired statistical power of 0.80, a minimum of 11 participants was required for each group. With this in mind, we recruited a total of 25 participants, expecting about a 10% drop-out rate. After receiving approval from the university ethics committee (PNUIRB/2019-64-HR), females aged 65 to 85 years, who agreed to participated in the study. All participants <Table 1> completed a Physical Activity Readiness Questionnaire prior to the start of the experiment to ensure the recruits could participate without any difficulties. Also any participants that provided any answer that indicated that participating could cause adverse problems were excluded and referred to an MD for a check-up. Any participants that had medicines that affected their physiological response to physical training and those with blood pressure medication were excluded from the study. Participants were randomly assigned to two groups: the exercise group (n = 13) and the control group (n = 12). Among the 25 participants in this study, three dropped out (one due to moving residence, another due to hospitalization, and the last for personal reasons), so the final number of participants was 22, 11 for strength training and 11 for the control group.
Measurements
Measurements were performed before and after the 20 weeks of SSEP. Blood pressure and HR were measured in the morning between 9and 10am after 30 min of resting before and after strength exercise program. Blood pressure was measured twice, and the average systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse pressure (difference between systolic and diastolic blood pressure) and heart rate (HR) were calculated. For blood testing all participants were instructed to fast for 12 h before the samples were taken. All blood samples were collected between 9 and 10 am by a certified nurse. The blood levels of homocysteine, TC, blood lipid profiles, TG, and ESR were analyzed from the blood samples. For homocysteine, TC, TG, and ESR, the venous blood was collected into a serum separation tube (SST), clotted at room temperature for 30 min to 1h, centrifuged at 3,000 rpm (or 3,500 × g) for 10 min, then the supernatant is transferred to the SST (5.0 mL) and stored below -20°C. Homocysteine analysis was performed using Architect i2000SR (Abbott, USA) with a Chemiluminescence Microparticle Immunoassay (CMIA). The blood levels of homocysteine, TC, blood lipid profiles, TG, and ESR were analyzed. To evaluate functional fitness, the senior fitness test which was validated by Rikli and Jones (19) consists of the following tasks 30-sec arm curl, 30-sec chair stand, back scratch, chair sit-and-reach, 2.44-m up-and-go, 2-min step test were tested.
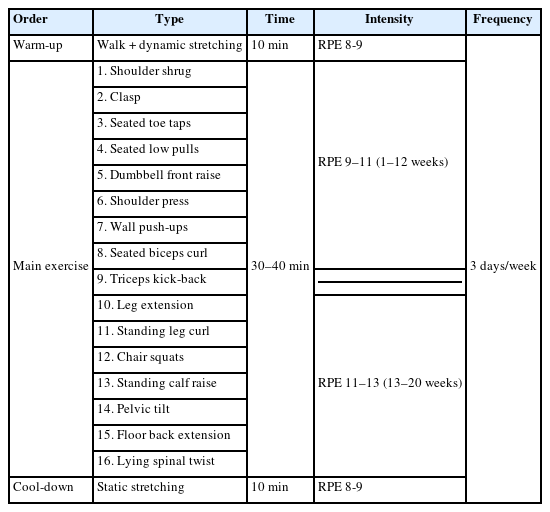
Exercise prescription
For this study, we developed a low level intensity strength exercise program for the older female population to include a full body workout, upper and lower body. This exercise program consists of 16 exercises and uses plastic bottles as weights for convenience<Appendix 1><Figure 1>. To learn and understand the SSEP, the participants had a 2-week adjustment period. SSEP was done three times per week for 20 weeks. A plastic bottle was filled with water up to the 500 mL (500 g) mark for weeks 1-6, 700 mL (700 g) for weeks 7-12 weeks, and 1000 mL (1kg) for weeks 13-20. Participants carried out the exercise program with the goal of increasing blood supply to the target muscles through soft, smooth, and accurate movement repetition rather than lifting heavy weights [20, 21]. After a 10-minute warm-up (dynamic stretching for the whole body), the intensity was monitored and controlled using rating of perceived exertion (RPE) 9-13 (light-little hard) in accordance with American College of Sports Medicine guidelines [22], with a 10-minute cool down (static stretching) to finish <Table 2>. The RPE of the participants was checked, periodically, during the main exercises to ensure that the participants did not feel overwhelmed and to ensure that the participants maintained the recommended exercise intensity. Individual RPE values were not recorded, however, the perceived intensity of the exercise was checked to be following the guidelines and program shown in <Table 2>.
Statistical Analysis
Statistical Package for the Social Sciences (SPSS, ver. 25.0) was used to calculate the mean, standard deviation, and independent t-tests were applied to verify homogeneity between the two groups. Paired t-tests were used to identify differences between times in each group. Two-way repeated measures ANOVA was applied to identify the interaction between group and time. Statistical significance was set at p<0.05.
Results
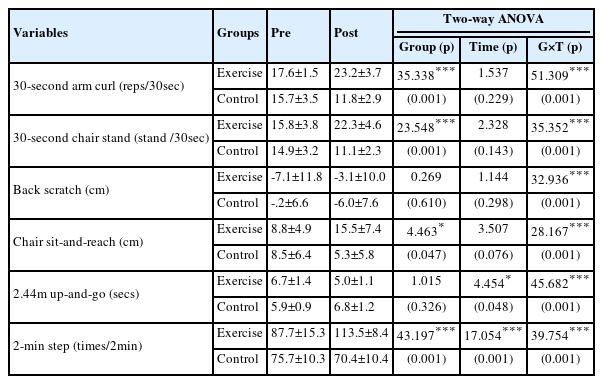
A two-way repeated measures ANOVA showed an interaction between groups according to time for homocysteine, SBP, HR and pulse pressure. There was a significant difference according to time for each group for the homocysteine, DPB, and HR. Whereas there were no other significant differences for the other variables<Table 3>. The senior fitness test results show there were interactions between group and time for all test items. <Table 4>.
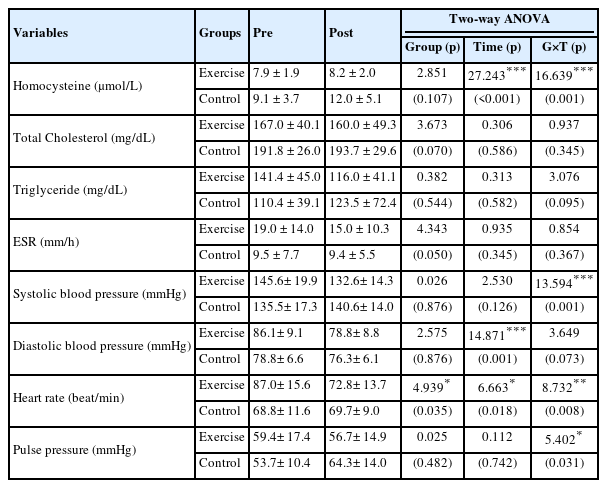
Changes in the level of blood, SBP, DBP, HR, and pulse pressure tests in the strength exercise and control groups
Discussion
There was a significant difference in the interaction (p=0.001) between the group and the time for the homocysteine. Additionally, there was a significant difference between the pre and post testing of both groups, with a significant increase in the exercise and control group (p=0.001). Steenge et al. [23] reported a significant decrease (p<0.05) in homocysteine concentration after 8 weeks of resistance exercise in adult men. Similar to the results of this study, Hur [24] reported the concentration of homocysteine after aerobic exercise for 12 weeks decreased (p<0.05) from 14.39±2.58 to 11.98±1.72 μmolL in the exercise group and increased from 13.53±2.12 to 14.93±2.17μmolL in the control group. Meanwhile, Guzel et al. [25] reported a significant increase (p<0.05) in blood homocysteine concentration after 12 weeks of callisthenic exercise in middle-aged women. There are contradictory results between other studies that seem to be due to differences in participants’ age, weight loss caused by training, frequency, intensity, type and time per session, and overall training period [26].
There were no statistical differences found between groups for TC levels (p = 0.070) and pre- and post-TC levels for both groups (p = 0.586). Based on a systematic research [27] examining dietary factors that may affect TC levels, the importance of diet is highlighted as being required for significant changes in TC levels agrees with our results not showing a significant difference. Similar to the TC, the TG data shows no significant differences (p=0.544). Data showed no significant difference (p=0.050) between groups for the change in ESR, with no interaction between group and time. There were no significant differences in the ESR levels in the exercise group 19.0±14.0 to 15.0±10.3 mm/h with no difference also for the control group (p=0.345) 9.5±7.7 to 9.4±5.5 mm/h. ESR tends to increase with age and is found to be higher in women than in men [28] and it has also been reported participants with high levels of regular exercise are associated with lower levels of ESR [29], which this study cannot support. In previous studies, there was no significant difference in SBP and a significant decrease (p<0.05) in DBP after performing compound exercise for older population [33], however, in our study, while there was no significant interaction, there were significant differences (p<0.05) in the changes between times for the exercise group for DBP. In contrast, there was an increase in SBP in the control group which shows a trend of increasing pulse pressure which is associated with an increase in rigidity of blood vessels [4]. Pulse pressure is an important risk factor for the incidence and mortality of cardiovascular diseases [5]. Increases in pulse pressure should not be overlooked, as it shows a change in arterial stiffness [31]. In this study, pulse pressure decreased (p<0.05) from 59.6 to 53.8 mmHg in the exercise group and increased (p<0.05) from 56.7 to 64.3 mmHg in the control group, with a statistically significant interaction (p=0.031). In relation to this, Moreau et al. [32] reported that hypertension among the older population requires effective treatment not only for blood pressure but also for control of pulse pressure. Moreau et al [32], recommended exercise as a treatment that effectively alters arterial extensibility and elasticity, reducing pulse pressure.
This study showed a significant interaction (p<0.05) after participating in SSEP; the resting heart rate decreased (p<0.05) in the exercise group and increased (p<0.05) in the control group. The change in HR in the older due to exercise training may be the main reason for the activation of cardiac vagus activities, similar in young people. Our results are similar to those of previous studies showing that strength exercise has a positive effect on blood pressure in older people and plays a role in improving cardiopulmonary function [16]. The majority of previous research focusing on improving resting heart rate has implemented aerobic training, but this study shows the effects of resistance training as another form of exercise that can positively reduce heart rate and improve cardiovascular function.
Our results showed all six tests confirmed significant positive effects (p<0.05), especially the results of the back scratch test are worthy of note. We think that, by repeatedly performing shoulder shrugs using the rhomboid, deltoid, and trapezius muscles simultaneously, a large amount of blood and oxygen was supplied to the muscles in the shoulder girdle, reconstitutes the muscle functions required for activities of daily living. The results of this study highlight the functional benefits of the SSEP for older women.
This study focused on female participants only due to their associated muscle loss due to aging [16] and different hormonal changes from the older male population. The study was performed for 20 weeks however; longer term effects should be studied in the future to see how long the effect may last and if continued strength training could maintain both muscle and a more efficient cardiovascular system. Future studies, should include the control of participant’s diet as this may negatively affect many of the variables.
Conclusions
The data reported shows that a low intensity SSEP significantly improved functional fitness (p<0.001), and had positive effects on cardiovascular fitness related variables, such as blood composition, blood pressure, HR, and pulse pressure (p=0.031). This study suggests low intensity resistance training may be an effective complementary maintaining method for cardiovascular functioning in the older female population. In particular, the measured blood indicators, blood pressure, HR, pulse pressure, and homocysteine levels improved (p<0.001), suggesting that light strength training can be a helpful strategy for optimal health care in terms of disease prevention for the older female population.
Acknowledgements
This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea(NRF-2019S1A5B5A07091375). I would like to thank Minji Park from the Department of Design, Pusan National University, for the artwork for figure 1.
Notes
The authors declare no conflict of interest. The founding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
References
Appendices
Appendix 1. Detailed explanation of SSEP exercises
- Shoulder shrug: Hold a plastic bottle in both hands and shrug one‘s shoulders. This movement is very important for shoulder flexibility, and the weight is loaded to the rhomboid muscle. The weight then moves to the middle trapezius and deltoid muscles. A large amount of blood is sent to the shoulder rotator muscle, which supports the movement of the shoulder.
- Clasp: Repeat clasp in a seated position. Start with 20 repetitions and increase as much as possible. This exercise stimulates blood to the antebrachial muscles and supports the movement of the wrist joints.
- Seated toe taps: Repeat toe taps in a seated position. Start with 20 repetitions and increase as much as possible. It increases the range of motion of the ankle joints.
- Seated low pully: Sit down facing your exercise partner, then pull each other’s hand. It is important to remind the participant to sit straight and focus on using the latissimus dorsi and rhomboid muscles. Additionally, instruct the participant to relax their arm, not pull by hands but use the elbow, and focus only on the latissimus dorsi and the rhomboid muscles to contract and relax.
- The dumbbell front raises: From a seated position, hold a plastic bottle in both hands and lift upward with the back of the hands facing up. Elbows should be slightly bent, and the resistance should be felt in the deltoid muscles.
- Shoulder press: From a seated position, hold a plastic bottle in both hands and press it above your shoulder. To smooth the press movement, take a front press position. Instruct the person to press with the elbow instead of pressing with the hand so as to transmit the resistance to the deltoid muscle effectively.
- Wall push-ups: Push up against the wall while in a standing position. When pressing against the wall, it is important to feel resistance to the pectoralis. Begin with seven repetitions and increase daily, if possible.
- Seated biceps curl: In a sitting position, hold pet bottles in both hands and curl both arms from elbows. When curling with the strength of the wrist, resistance must be transferred to the biceps brachii muscle. Curl both arms following a semicircle to ensure that there is continuous resistance in the biceps brachii muscle. Triceps kick-back: In a sitting position, hold pet bottles in both hands and stretch arms backwards. To increase tension in the triceps brachii muscle, the participant bends the wrist forward while holding the plastic bottles.
- Leg extension: Perform leg extension on each leg by turning in a sitting position with plastic bottles tied to ankles. When performing extension of the quadriceps femoris group, remind the participant to focus on transferring the resistance to the vastus medialis, vastus lateralis, vastus intermedius, and rectus femoris. In full extension, flex the knee slightly while raising the leg and hold for 2–3 sec to completely contract the muscles.
- Standing leg curl: Plastic bottles are tied to both ankles. In a standing position, the foot is curled around the knees as a pivot. This curling the foot around the knee maximizes resistance to the hamstring by moving the foot in a semicircular shape.
- Chair squats: Sit on the chair with plastic bottles in both hands, like in a front squat position. It is recommended that this be done after sufficient warm-up of the hip, knee, and ankle joints.
- Standing calf raise: Stand on your toes holding the plastic bottles to your side. Bend your knees slightly while you rise and ensure that the resistance is concentrated on the gastrocnemius muscle. It is vital to maintain the knee only slightly bent as though the knee stretches out, then the resistance will be transferred to the upper leg muscles.
- Pelvic tilt: Lying on the floor, push the pelvis up from the supine position. Ensure that the person focuses on using their core (abdominals and erector spine muscles) and gluteus maximus muscles.
- Floor back extension: Lie down on the ground, raise the right arm with the left leg then return to base position; then raise the left arm and right leg. This can then be increased in difficulty by raising the legs and arms simultaneously.
- Lying spinal twist: From a supine lying position straighten right leg and bring the left to the hip at a right angle, then rotate the left leg to the right side. Hold the stretch for 10–20 s, return to the center position, change the legs, and rotate to the left side with the right leg.